Patient Handover from the Emergency Department
Patient handover from the Emergency Department (ED) nurse to the Southern Intensive Care Unit (ICU) nurse
The ED and ICU have been looking at ideas to improve the patient handover process and satisfaction between nursing staff. Patient handover from one unit to another represents a vulnerable time for communication of patient information. Both areas are fast-paced, unpredictable and clinical information can be lost during the patient handover process. The plan is to standardise the handover process, similar to the current process for cardiac surgery patients returning to the ICU, and use a handover tool.
The future plan for ED to ICU patient handover:
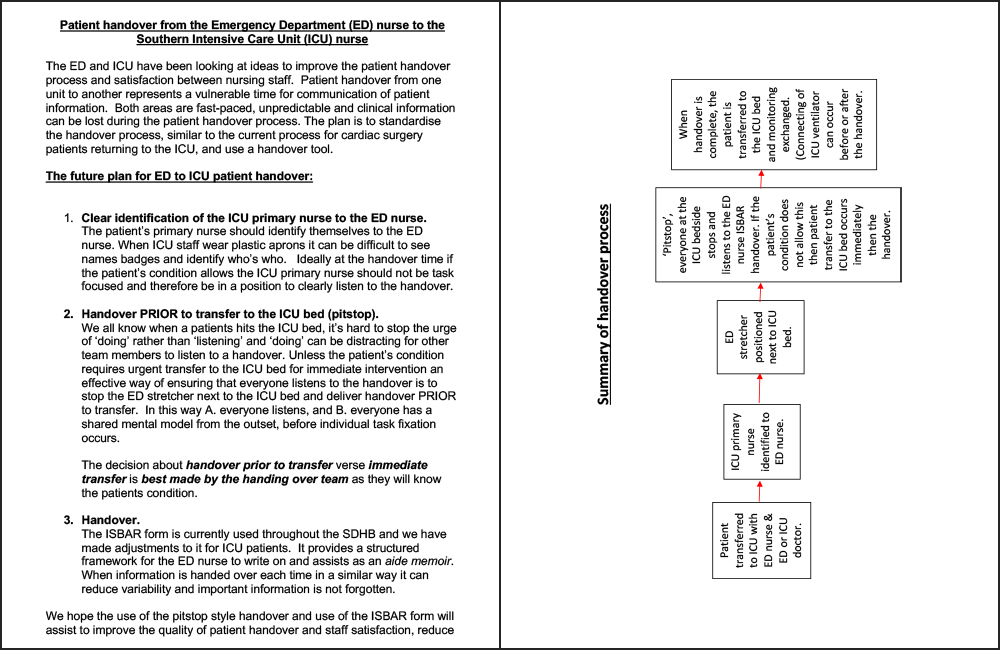
- Clear identification of the ICU primary nurse to the ED nurse.
The patient’s primary nurse should identify themselves to the ED nurse. When ICU staff wear plastic aprons it can be difficult to see names badges and identify who’s who. Ideally at the handover time if the patient’s condition allows the ICU primary nurse should not be task focused and therefore be in a position to clearly listen to the handover. - Handover PRIOR to transfer to the ICU bed (pitstop).
We all know when a patients hits the ICU bed, it’s hard to stop the urge of ‘doing’ rather than ‘listening’ and ‘doing’ can be distracting for other team members to listen to a handover. Unless the patient’s condition requires urgent transfer to the ICU bed for immediate intervention an effective way of ensuring that everyone listens to the handover is to stop the ED stretcher next to the ICU bed and deliver handover PRIOR to transfer. In this way A. everyone listens, and B. everyone has a shared mental model from the outset, before individual task fixation occurs.
The decision about handover prior to transfer verse immediate transfer is best made by the handing over team as they will know the patients condition. - Handover.
The ISBAR form is currently used throughout the SDHB and we have made adjustments to it for ICU patients. It provides a structured framework for the ED nurse to write on and assists as an aide memoir. When information is handed over each time in a similar way it can reduce variability and important information is not forgotten.
We hope the use of the pitstop style handover and use of the ISBAR form will assist to improve the quality of patient handover and staff satisfaction, reduce variability, potential loss of information and result in improved quality of care and ultimately patient safety. Future feedback on the form and handover process will be sought for ongoing development.
Specifications
- Last Updated: 2019
- Author(s): Southern District Health Board, New Zealand
- Category: Guidelines
- Tags: 2019, English, New Zealand National Clinical Network, Southern District Health Board
Word Documents
Please login to access file downloads.
PDF Documents
Please login to access file downloads.
